Why the gut-brain connection matters
We’ve all felt the gut-brain axis. You get “butterflies” before a big presentation. You trust a “gut feeling” even when your brain can’t explain why. Your stomach “knots up” when stress takes over.
This constant conversation between the digestive system and the nervous system runs so deep it has shaped our language, revealing how naturally we link emotions to digestion. And today, research is showing just how intricate that connection truly is.
At Throne, we believe this matters because your gut health influences how you feel, think, and function every day. By making those invisible patterns visible, you get the chance to better respond to your body’s signals.
Ancient roots of the gut-brain idea
Long before modern science, physicians and philosophers noted that the gut and mind seemed to move together. Ancient Greek texts described the “sympathy” between the stomach and the brain, observing how fear or grief could disrupt digestion. In traditional Chinese medicine, the stomach and spleen were thought to influence not only physical nourishment but also mental clarity and worry. Ayurvedic practitioners in India similarly emphasized how imbalances in digestion could manifest as disturbances in mood and perception.
Taken together, these traditions reveal that the gut-brain axis isn’t a particularly modern discovery – it’s an ancient intuition, recognized across cultures long before we had the tools to prove it.
The modern discovery of the gut-brain axis
The scientific exploration of the gut-brain axis accelerated in the 20th century. A pivotal early milestone came in 1904 with Ivan Pavlov’s Nobel Prize-winning experiments, which demonstrated how psychological cues like anticipation could trigger digestive responses such as salivation and gastric secretions.
Central to this axis is the vagus nerve, the body’s longest cranial nerve. Modern physiology has shown how it serves as a two-way highway, relaying sensory information from the gut to the brain and regulatory signals back, modulating everything from heart rate to intestinal motility.
In parallel, scientists uncovered the gut’s surprising role in neurotransmitters. In the 1930s, Italian pharmacologist Vittorio Erspamer identified serotonin in enterochromaffin cells, and by the 1950s, it was established that about 90–95% of the body’s serotonin is produced in the gut. But this serotonin largely regulates gut motility—it doesn’t cross into the brain.
Later, researchers such as Michael Gershon revealed how gut microbes also influence neurotransmitters like dopamine and GABA, molecules that affect anxiety, motivation, and calm.
The latest science
By the early 2000s, landmark studies made the axis measurable. A 2004 mouse study showed that germ-free animals had exaggerated stress responses, which normalized when colonized with Bifidobacterium infantis (Sudo et al., 2004). Later reviews by Cryan and Dinan mapped the many routes of influence—through immune signaling, vagal pathways, and microbial metabolites.
Stress also acts in the opposite direction: psychosocial stress can increase intestinal permeability, sometimes called “leaky gut,” fueling inflammation.
Clinically, this shows up in conditions like IBS, which has strong links to anxiety and depression. Emerging evidence even suggests the gut may play a role in Parkinson’s disease, though this research is still early.
What’s clear is that this axis is not a simple on/off switch—it’s a dynamic, ongoing conversation. Every meal, every stressor, every night of sleep nudges the balance.
Clearing up misconceptions
With so much buzz around the gut-brain axis, some myths are worth addressing.
Myth 1: “The gut controls the brain’s serotonin supply.”
It’s true the gut produces most of the body’s serotonin, but gut-derived serotonin doesn’t cross the blood-brain barrier. Its influence is indirect, mediated through nerves and immune signals—not as a direct fuel for mood in the brain.
Myth 2: “Probiotics can cure depression.”
Some studies suggest certain strains may help with mood or stress, but the effects are modest and vary by individual.
Listening to your gut with Throne
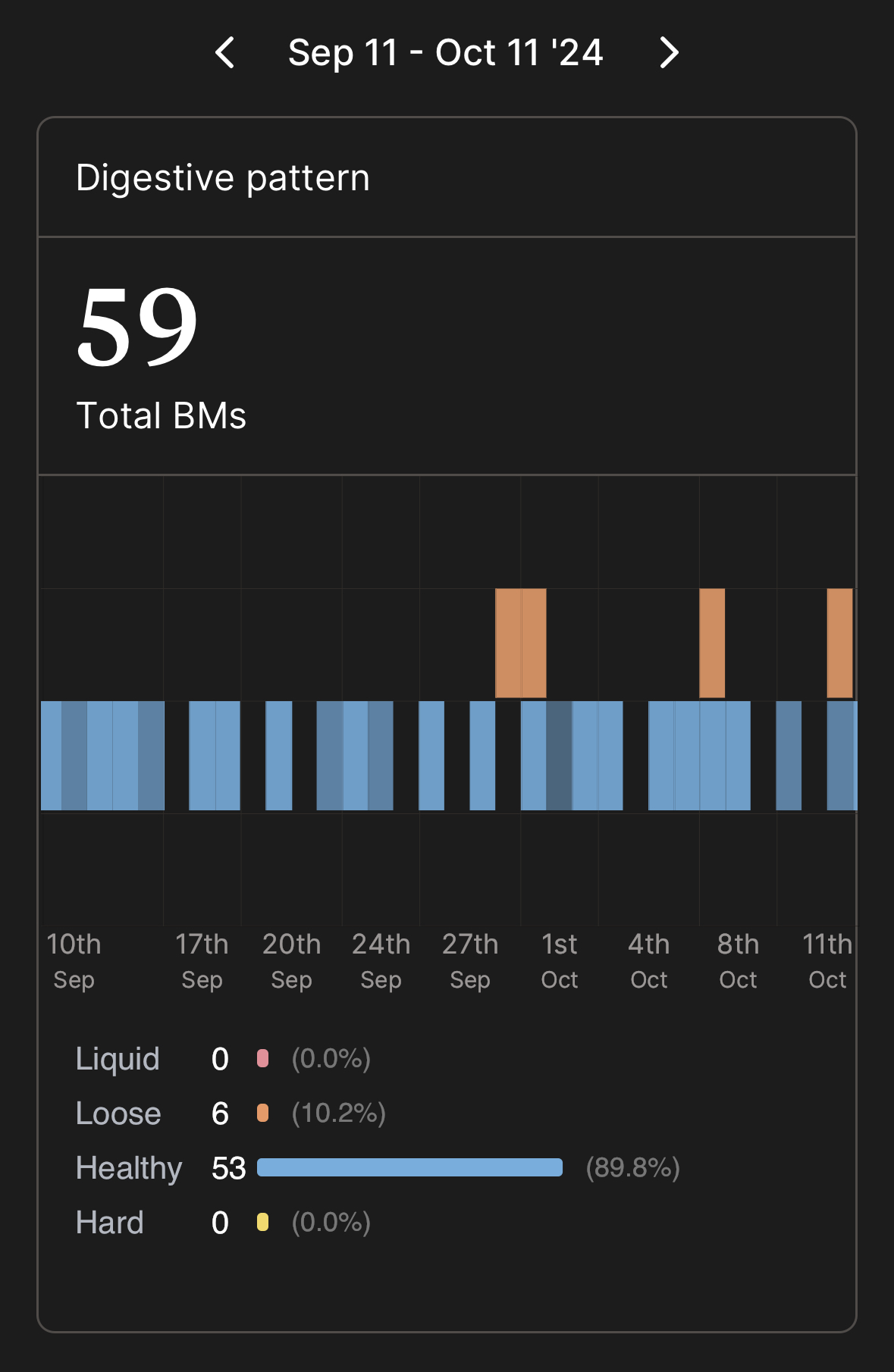
We’ve already seen the gut-brain axis in our own Throne data. Pictured below is a relatively low-stress month, note the consistent healthy poops:
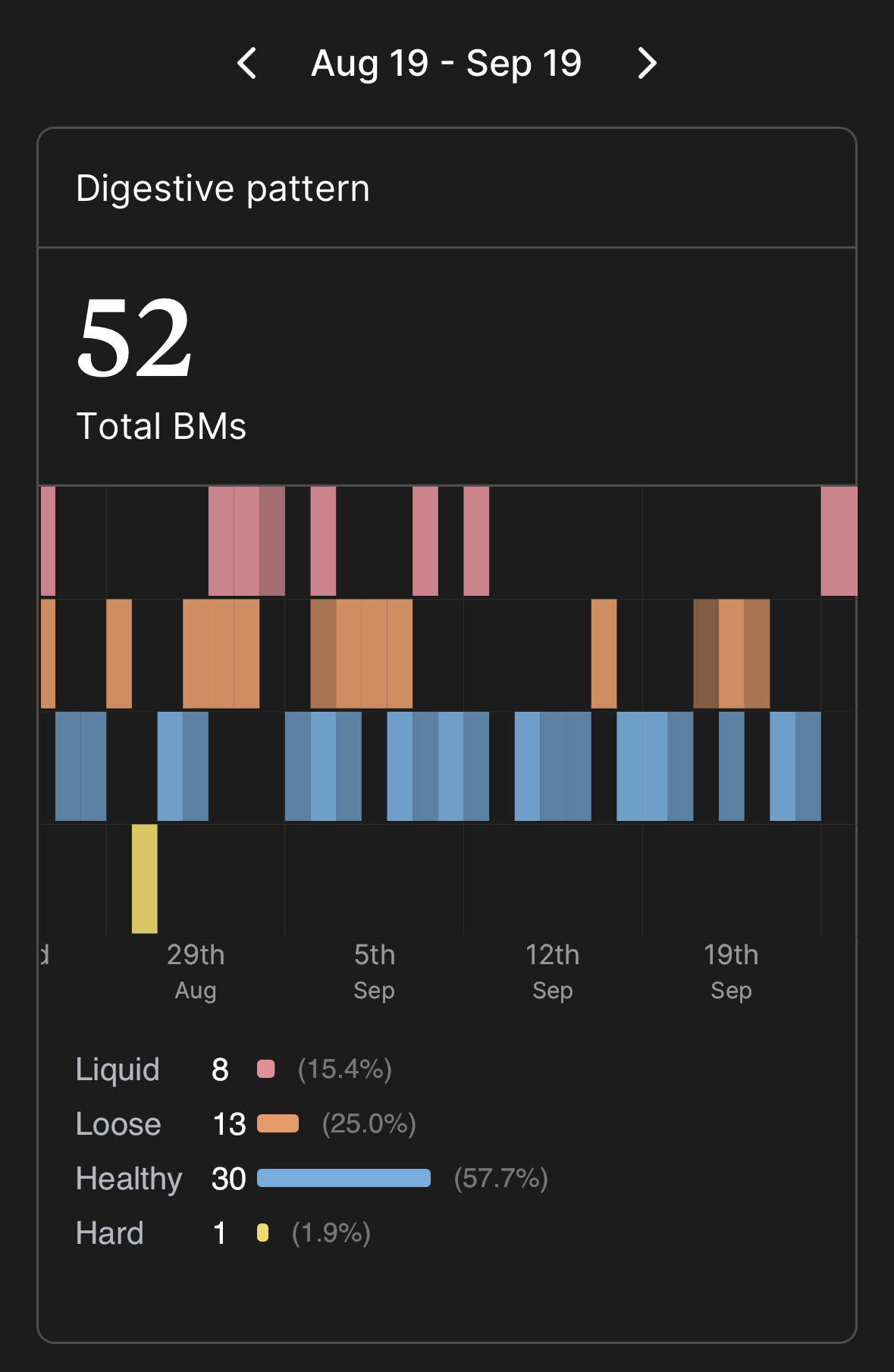
And here is what a high-stress month looks like going into a big launch:
Throne exists to make this invisible dialogue more visible. By tracking digestive patterns, Throne helps you “know your normal” with effortless, daily insights. That awareness is the first step in supporting both gut health and mental well-being.
Your gut is talking to your brain all day long. With Throne, you can finally listen in.
This article is for informational purposes only and is not intended to provide medical advice. Throne is not a medical device and does not diagnose, treat, cure, or prevent any disease.